Bladder Conditions
Disorders of the bladder can significantly impact daily life and may present with symptoms such as frequency, urgency, waking at night to void (nocturia), slow flow, incontinence or difficulty urinating.
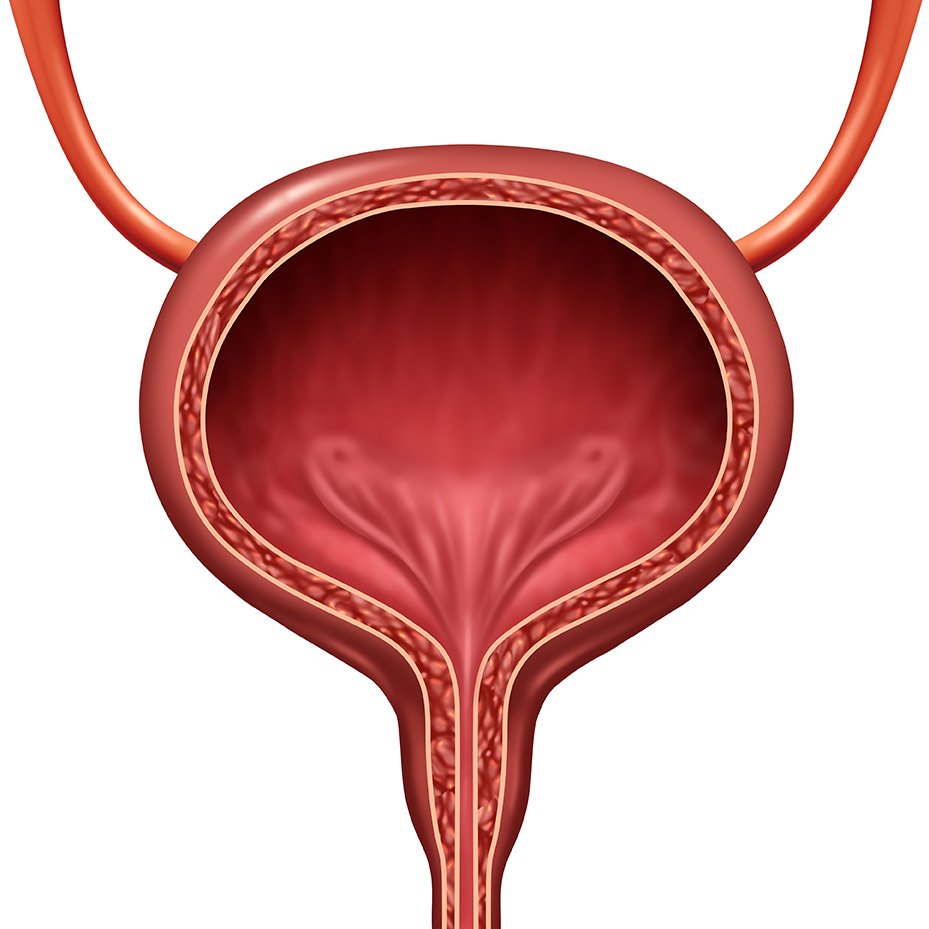
The bladder plays a vital role in storing and releasing urine. Dr. Basto specialises in managing conditions of the bladder such as recurrent urinary tract infections (UTIs), lower urinary tract symptoms, incontinence and haematuria (blood in the urine).
Conditions treated by Dr Basto
Recurrent Urinary Tract Infections (UTI)
UTIs are common and can significantly affect quality of life causing pain, frequent urination and blood in the urine. Around 50-60% of women will experience a UTI in their lifetime, with men also affected, particularly with age. When UTIs become recurrent it can impact your work, personal life and mental health. By the time patients make it to a Urologist they have usually had many . Some patients develop a ‘sensitised’ bladder.
At your consult, Dr Basto will take the time to explore your history, urine culture results and previous investigations. In recurrent cases, evaluation with a cystoscopy may be necessary to identify underlying causes. Dr Basto will guide you through the current evidence for prevention and treatment of your UTIs.
Advanced therapies such as immunoprophylaxis show very promising results and their use is rapidly expanding. An example of immunoprophylaxis is the UTI vaccine Uromune (MV140) which contains inactivated bacteria of the four most common organisms to cause UTIs. This causes the body to mount an immune response which acts at the bladder to fight off future infections.
Please book a consult with Dr Basto for further assessment and discussion of your recurrent UTIs.
Urinary Incontinence
Urinary incontinence refers to the involuntary loss of urine, affecting daily activities and quality of life. It may range from mild leaks to complete loss of bladder control. There are three main types of incontinence including urge incontinence, stress incontinence and overflow incontinence. The underlying cause can sometimes be difficult to determine from history alone, as the symptoms often overlap. Specialised tests are frequently required such as a cystoscopy (to assess your anatomy) or a urodynamics assessment (to assess your bladder function).
Treatment strategies are targeted to the underlying cause. Dr Basto will discuss relevant non-surgical and surgical treatment options that are suited to your individual situation. Surgical options for urge incontinence include sacral neuromodulation and bladder injections E.g botox to relax the bladder. Surgical options for stress incontinence include peri-urethral bulking agents and urethral sling procedures. For treatment of overflow incontinence, refer to ‘Urinary retention’ below.
Lower Urinary Tract Symptoms
Lower urinary tract symptoms (LUTS) encompass issues such as frequent urination, urgency, slow urinary flow and nocturia (night-time urination). These symptoms can result from prostate conditions, bladder dysfunction or other urological and non-urological issues.
Specialised tests are frequently required such as a cystoscopy (to assess anatomy) or a urodynamics assessment (to assess bladder function). Treatment options might include medications, bladder training and/or minimally invasive procedures. Dr Basto will tailor your management to the underlying cause.
Urinary Retention
Urinary retention occurs when the bladder does not fully empty, leading to discomfort, urinary tract infections and kidney problems. Acute cases may require immediate catheterization, while chronic cases may be treated with behavioural modifications, catheters or surgery to relieve obstruction and/or restore normal bladder function. Sacral neuromodulation can help to restore bladder emptying in some patients.
Neurogenic bladder
Neurogenic bladder occurs due to neurological conditions like spinal cord injuries, multiple sclerosis or Parkinson’s disease. Symptoms may include urinary incontinence or retention. Urodynamic assessment is usually required due to the more complex nature of the bladder dysfunction.
Treatments are then tailored to the individual's needs and may involve intermittent or long-term catheterization (Such as a suprapubic catheter), oral medications, or surgeries such as Botox to the bladder or sacral neuromodulation. Less commonly reconstructive surgery to improve bladder function and quality of life are required.
Haematuria (Red blood cells in the urine)
Haematuria refers to the presence of blood in the urine and can indicate serious conditions such as infections, kidney stones or cancers. Evaluation involves imaging, urine testing and cystoscopy to identify the cause. Treatment depends on the underlying condition and aims to address the root cause and prevent recurrence.
Sterile pyuria (White blood cells in the urine)
Sterile pyuria refers to the presence of white blood cells in the urine without evidence of a bacterial infection on urine culture. It can be a sign of various underlying conditions, including stones, infection, inflammation or less commonly (but importantly) cancer. Proper evaluation may involve urine testing, imaging and cystoscopy to identify the cause.
Bladder pain syndrome
Bladder pain syndrome (BPS) can cause chronic pelvic pain, pressure or discomfort related to the bladder, often accompanied by urinary urgency and frequency. The exact cause is unknown, but it can severely impact daily life. It is important to exclude all reversible causes, as such evaluation with a cystoscopy is often required.
Management generally requires multiple treatment approaches such as behavioural and lifestyle changes, preventing UTIs, medications, bladder instillations, nerve stimulation therapies or bladder botox. Holistic multimodal care in combination with a psychologist or pain specialist is often recommended.
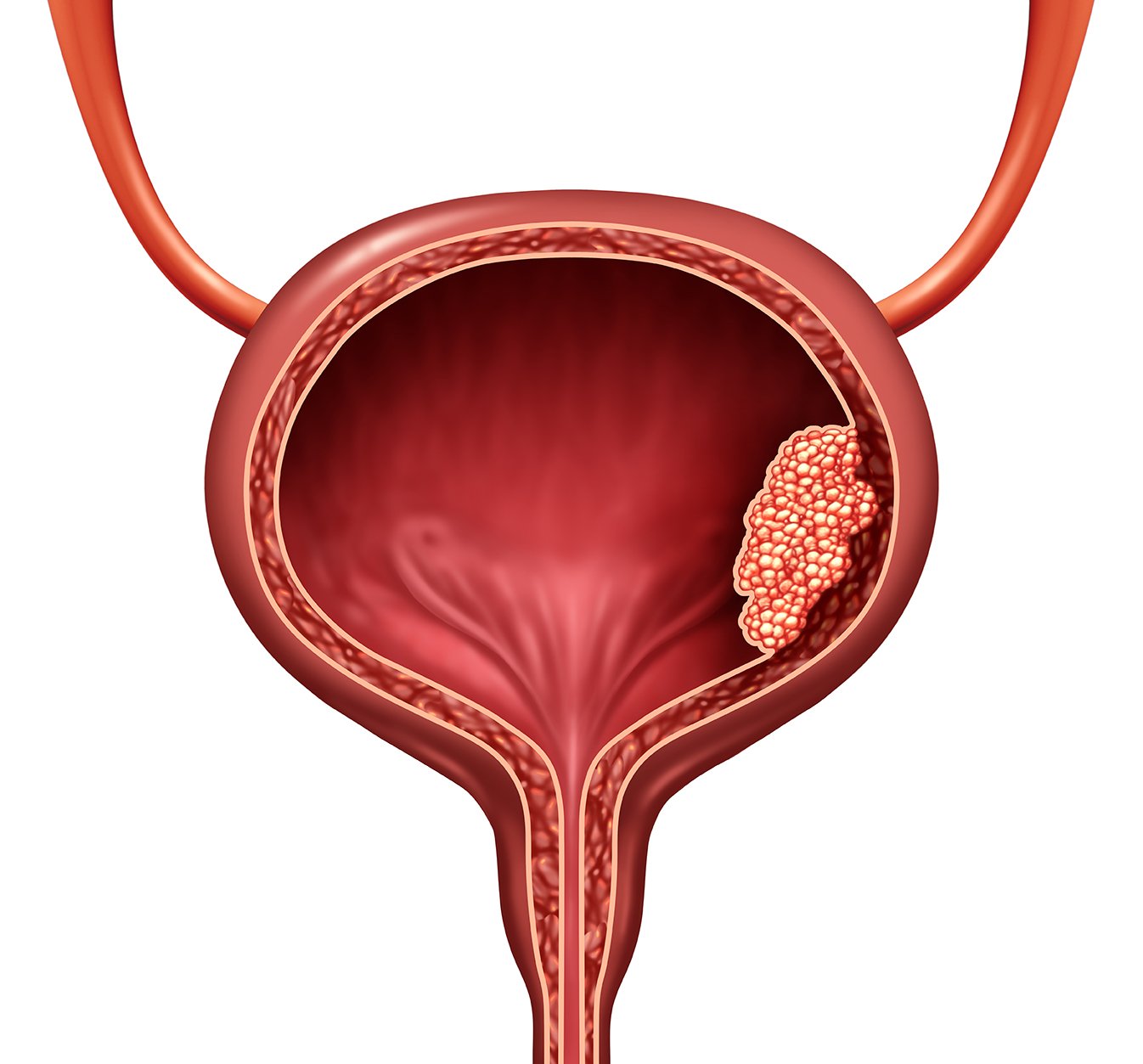
Bladder Cancer
Bladder cancer often presents with blood in the urine. Treatments depend on the stage and may include transurethral resection (TURBT), intravesical therapies, cystectomy (partial or complete bladder removal) and advanced systemic therapies.
As a reconstructive and functional urologist, Dr Basto specialises in restoring anatomy and function of the urinary tract. She manages early stages of bladder cancer diagnosis and management. For more advanced stages of cancer or complex cancer surgeries, she works closely with trusted uro-oncology colleagues who have specialized expertise in these areas. This collaborative approach ensures that patients receive the highest standard of care tailored to their individual needs, whether in the early or advanced stages of cancer.
Restorative Urology Sydney
Providing compassionate care to all her patients, Dr Marni’s priority is to restore function & improve your quality of life.